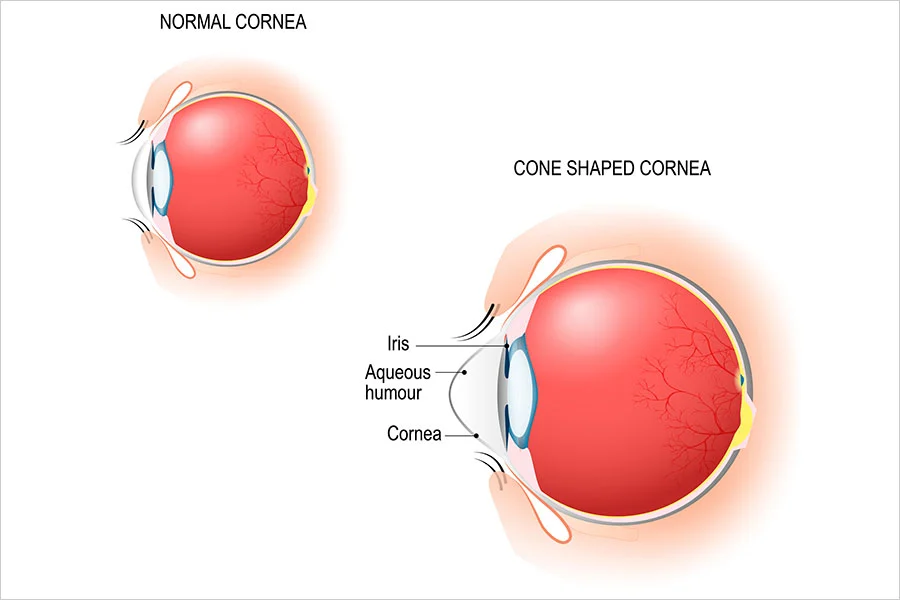
New Zealand has the second highest rate of keratoconus diagnoses in the world. This progressive condition is characterized by an unusually thin cornea bulging into an irregular cone shape. It causes distorted and blurred vision in patients, even if they wear glasses
Keratoconus commonly develops in patients who frequently rub their eyes, like those with allergies and eczema. It’s also genetic, meaning those with a family history and Maori or Pacific Island descent are at a higher risk for the condition.
After a preliminary eye exam, we diagnose keratoconus with a corneal topography, looking out for cones, scarring, and other abnormalities. It’s most commonly diagnosed between the ages of 20 and 30 years old and though it presents in both eyes, it’s often worse in one than the other.
Once we determine the severity of your condition, we’ll discuss all of the treatment options available to you. These are the most common treatment courses:
Are you legally blind if you have keratoconus?
It does not typically lead to blindness if treated early on with RGP. But in a small percentage of cases with permanent corneal scarring, severe vision loss is possible.
Can keratoconus be corrected?
Though it cannot be permanently corrected, mild to moderate keratoconus can be treated with RGP lenses or even eyeglasses in extremely mild cases.
Is keratoconus a serious disease?
Yes. If left untreated, it can lead to permanent vision loss. It’s important to see an optometrist as soon as you notice vision issues.
Can I live a normal life with keratoconus?
With help from Curtis Vision optometrists, you’ll be able to live a happy, healthy, and normal life with keratoconus.
 Book An Eye Test
Book An Eye Test